Diabetic Foot Assessments
Diabetes is a complex disease that can affect many parts of your body, including your feet. In relation to the feet, diabetes can cause two main problems:
- Loss of sensation (nerve damage or peripheral neuropathy)
- Restricted circulation and blood flow (peripheral vascular disease)
This means that people with diabetes may not feel (or ‘sense’) the symptoms of foot problems. And foot injuries or infections may take longer to heal due to reduced blood flow or may not heal at all. This can cause long-standing foot ulcers and even amputations.
This is why the Who (world health organisation) and Podiatry Ireland Council (MPI) and the International Working Group on the Diabetic Foot (IWGDF) recommend that all diabetic patients have their feet assessed by a qualified podiatrist at least every 12 months so that any changes can be managed and addressed as soon as possible. (The frequency of these assessments may change depending on your foot health).
What is involved in a Diabetic Foot Assessment
As part of your diabetes risk assessment, your podiatrist will usually begin by asking a few questions about the management of your diabetes and feet. Your podiatrist will then look at each of the following systems to gain an overall understanding of your foot health and your risk of diabetic foot complications such as ulcerations and amputations.
Vascular assessment
A vascular assessment will look at the blood supply to your feet. Good blood supply is vital for good foot health. If the arteries to your feet are affected by diabetes then your feet will not get the ‘nutrients’ they need from the blood. This can cause your skin to become dry, your nails can become brittle, and the hair on your feet and legs can stop growing.
More importantly, without good blood flow to the feet any cuts, scrapes or injuries will be much slower to heal, and your body will have a hard time fighting off infections. In extreme cases, if the blood supply to the feet is so poor the skin may start to breakdown, ulcerate and even develop gangrene!
Diabetes and feet swelling can also occur, as fluid can accumulate in the feet and ankles when the blood does not circulate properly.
In order to assess your vascular system your podiatrist will do the following
- Determine if they can feel the pulse in your feet
- Use a Doppler ultrasound machine to assess the health and the condition of the arteries in the feet
- If required, they may perform a Toe Pressure Analysis to determine the blood pressure and bloody supply to the toes
- Assess the overall appearance of the feet by looking at the colour of the skin, temperature of skin, texture of the skin and presence of hair.
Neurological assessment
A neurological assessment involves looking at the health of the nerves in the feet. We rely on functioning nerves for feeling in our feet, to tell us what is going on with them. For example, if we step on a small rock, it is the nerves that detect this pain, which then tells us to remove the rock to eliminate the cause of this pain.
With diabetes the nerves become less responsive. This means that we may not feel the usual feelings in our feet. This often begins as feet tingling and feet numbness. This can progress to a stage where the feet are completely ‘numb’. This can lead to very serious complications through unknown injuries and damage to the feet.
To assess the condition of the nerves podiatrists generally do the following (don’t worry, its painless!):
- Use what is called a ‘10g monofilament’. This is not much more than a piece of fishing wire. With your eyes closed, the podiatrist will touch various places on your foot with this filament, to see if you are able to detect this very slight touch.
- We also use a ‘tuning fork’. This tuning fork is made to vibrate and is placed upon a bony prominence on your feet. This should send a vibration/ humming sensation through your feet. However if you are in the early stages on neuropathy, you may be unable to feel this vibration or this sensation may hang around for longer than the tuning fork is touching the skin. Both responses indicate to the podiatrist that there could be some issues with the nerves.
- Your podiatrist may also perform a few other tests to look at your ‘proprioception’. This is the understanding of your body’s position in space. If your proprioception is affected you may be at a higher risk of falls.
Dermatological assessment
This involves the podiatrist looking at your skin and nails. Your podiatrist may note some of the following:
- Corns & callus and thickened skin under your foot are sings that there is lots of pressure carried in this area. High-pressure areas in diabetic patients are worrying to a podiatrist as these areas are prone to skin breakdown.
- Heel fissures or cracks are not only painful but are also are a risk of infections for people with diabetes and feet issues
- Ingrown toenails are a nasty problem for anyone! But for people with diabetes, and ingrown toenail can become a serious concern.
- Diabetes and feet itching may be a sign of a tinea infection. This usually presents with flaky or splitting skin, especially around the toes. Treatment for tinea should begin promptly as secondary bacterial infections develop.
If your podiatrist notices any of these dermatological concerns they will do their best to treat them during the consult. For example, removing the corns or callus, parring back the fissured heels, cutting the nails safely etc.
Musculoskeletal and gait assessment
Your podiatrist will also look at your stance and the way that you walk. This will show if there are any ‘high-pressure’ areas under your foot, which may be prone to skin breakdown and ulceration. A gait assessment will also show how steady you are on your feet, and may reveal muscle weakness or show and if your balance is affected.
Footwear assessment
You podiatrist will also assess your footwear, so it’s a good idea to bring these to your appointment. Correct footwear is very important to prevent foot problems from diabetes. A good shoe will protect your feet and give you support and cushioning. Walking around barefoot will expose your feet to injury and a poorly fitting shoe can lead to pressure areas, blisters, sores and skin breakdown.
Your podiatrist can give you recommendations on the right type of shoe for you.
After this assessment is conducted your podiatrist will talk you through their findings and explain what it all means. They will answer any questions you may have and will advise on what you can do to look after your feet and reduce your chance of developing diabetic foot complications.
With your consent, we then pass on these findings from the diabetes risk assessment tool to your GP and complete a Type 2 Diabetes Risk Assessment Form if required.
We diagnose and treat the following diabetes related foot problems:
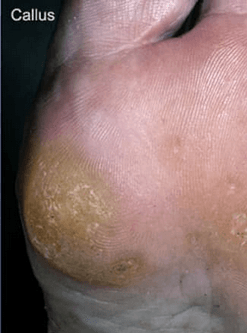
Calluses
Calluses (Hyperkeratosis) are a build up of thick skin on the foot caused by friction in high pressure areas of the foot. This complaint is often accompanied by corns and can be mildly uncomfortable to painful and debilitating.
Calluses often appear on the bottom of the foot around the forefoot, as well as the heel and around the sides and tips of the toes. If calluses are left untreated, they can interrupt the vascular blood supply to the area and ulceration may result.
It is recommended that people with diabetes are regularly screened and treated accordingly to prevent the development of a callus that can cause ulcerations.
We provide the following solutions:
● Complaint removal
● Advice to prevent the re-occurrence
of this complaint
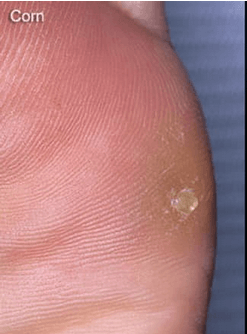
Corns
Corns (Heloma Dura and Heloma Molle) are painful lesions/spots of thickened skin on the foot caused by friction in high pressure areas of the foot.
Hard corns (Heloma Dura) appear on the top and sides of toes often secondary to footwear pressure and also along the bottom of the foot. Soft corns (Heloma Molle) in most cases appear between the fourth and fifth toes. These have an unbearable stinging sensation and are extremely uncomfortable.
If corns are left untreated, they can become very painful and may interrupt the blood (vascular) supply to the area and cause an ulcer. It is recommended that people with diabetes are regularly screened and treated accordingly to prevent the development corns that can cause ulcerations.
We provide the following solutions:
● Complaint removal
● Advice to prevent the re-occurrence
of this complaint
Ingrown toenails
An ingrown nail (Onychocryptosis) will occur when a portion of the nail forms a jagged edge (spicule) and begins to protrude into the surrounding tissue as the nail grows. Ingrown toenails are one of the most common reasons a client seeks the services of a podiatrist.
They may occur as a result of poor nail cutting, direct trauma to the area, running in poorly fitted footwear or they may be due to a genetic predisposition which means the nails are too wide or too curled (involuted).
Ingrown toenails should be treated as quickly as possible as infection often occurs. Whilst antibiotics may sometimes be required, they alone are generally not a long term solution for the problem. The nail spicule must be removed, as leaving it will not allow the wound to close and the area is likely to become infected or painful again.
We provide the following solutions:
● Removal of the spicule.
Following this, nail retraining is required to
help the nail grow out past the skin fold or
the problem will reoccur some months later. Thus, retraining of the problem nail is a vital part of solving the problem
permanently.
● In persistent and severe cases nail surgery
or a partial nail avulsion may be required. This is a minor surgical procedure conducted under local anaesthetic in the podiatry rooms. A narrow problematic
portion of the nail is removed using a
strong alcohol solution to prevent any nail
regrowth in the problem area. This is a
permanent solution and has a success rate
of over 95%.
● We also offer advice to prevent recurrence
of the problem.